Many experts say everyone will experience acne at some point in their lifetime. Although acne has been widely viewed as a cosmetic problem, studies have shown that it has profound impact on quality of life, self-esteem, and social functioning. Thankfully, recent research has led to a greater understanding of the genetic, environmental, and molecular events that contribute to its prevalence and severity.
There are now many safe and effective treatments for acne which target one or more of the four distinct but interrelated causes:
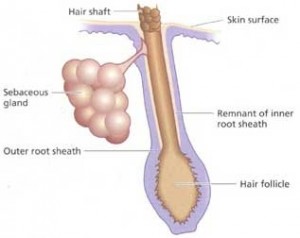
- Clogging of the hair follicle caused by overgrowth of the follicle surface cell skin layers.
- Increased sebum (oil-like product produced in hair follicles) production and clogging of the follicle by sebum. This is further increased in adolescence due to elevated hormone levels.
- Colonization and growth in the hair follicle by a normal bacterial inhabitant of the skin surface (Propionibacterium acnes, or P. acnes).
- Inflammatory response to the bacteria along with by-products of sebum breakdown.
Treatment. Acne is caused by a variety of factors and the severity between each patient varies widely. Therefore it is very important to discuss appropriate therapies with your child and pediatrician or dermatologist. Current guidelines for treating acne specify options for mild, moderate and severe disease and target one or more of the 4 causes. There is no accepted consensus on how to classify acne severity but it is loosely based on the number, type, and size of acne lesions.
Mild to Moderate. The mainstay of treatment is topical (on the skin) therapy – Agents used include retinoids, benzoyl peroxide, topical antibiotics, and sulfur-containing products.
For example, a typical topical skin regimen for mild acne might include benzoyl peroxide gel or wash followed by an antibiotic lotion applied. However there are many ways to combine treatments and often the best regimen is arrived by trial and error.
Moderate to Severe. If acne is unresponsive to topical treatments or if your child is developing cysts or scarring, more aggressive treatment is warranted. Options include oral medications including antibiotics or contraceptives or phototherapy. Use of any of these agents requires prescriptions and discussion with close observation by your pediatrician or dermatologist. The most common antibiotics used are tetracyclines, Bactrim (SMZ-TMP), and erythromycin with varying adverse effects associated with each.
Do’s and Don’ts for Acne-Prone skin
- Be consistent with your skin care routine.
- Moisturize your skin and protect it from the sun.
- Remove make-up before bed.
- Use oil-free makeup, concealer and skin care products and use a glycolic/salicylic acid-based cleanser.
- Do not pick at blemishes.
- Do not over scrub your face or exfoliate aggressively.
- Do not use soap on your face
- Do not use products for dry skin especially ones with oils, butters or waxes.
And again please remember to always discuss any new acne treatment with your pediatrician or dermatologist. If you need help finding a pediatrician or specialist, call the St. Louis Children’s Hospital Answer Line at 314.454.KIDS or 800-678.KIDS.
References:
Groff BM et al. Adolescent Acne. Consultant For Pediatricians. 2009;8:S3-19.
Tom WL, Barrio VR. New Insights into adolescent acne. Curr Opin Pediatrics. 2008;20:436-440.
Katsambas A. New and emerging treatments in dermatology: acne. Derm Ther. 2008:21:86-95.




Great article and very informative 🙂 I was curious on what sebum was after reading this and found this article which was informative https://www.mapleholistics.com/blog/no-secrets-in-sebum-sebum-defined/